|
Home > All Topics > Evidence-Based Management of Angioedema in Urgent Care (Pharmacology CME)
Evidence-Based Management of Angioedema in Urgent Care (Pharmacology CME)
Below is a free preview. Log in or subscribe for full access. Or, get a free sample article Evidence-Based Management of Angioedema in Urgent Care:
Search Log in Buy This Issue Subscribe
Table of Contents About This Issue When a patient arrives in the urgent care clinic with symptoms such as nonpitting edema, urticaria, pruritis, abdominal pain, and/or respiratory distress, angioedema is a primary differential diagnosis. While often localized and self-limiting, angioedema can quickly become a life-threatening emergency. Identification of the cause and thorough examination of the patient are crucial for appropriate management. In this issue, you will learn: The distinctive presentations and mechanisms of histamine-mediated, bradykinin-mediated, and idiopathic angioedema. How to be on guard for potentially life-threatening laryngeal swelling and/or anaphylaxis. The signs and symptoms that should prompt emergent transfer to the emergency department. The appropriate medications to effectively manage histamine-mediated angioedema, including epinephrine and antihistamines. The special considerations and management approaches for pediatric patients. Disposition decisions based on the type of angioedema, staging of the disease, and indications for observation. CODING & CHARTING: Coding for angioedema is highly variable and dependent on the cause and patient presentation. Learn more in our monthly coding column.
Table of Contents Introduction Etiology and Pathophysiology Histamine-Mediated Angioedema Bradykinin-Mediated Angioedema Hereditary Angioedema Acquired Angioedema Angiotensin-Converting Enzyme Inhibitor-Induced Angioedema Other Drugs Associated With Angioedema Idiopathic Angioedema Differential Diagnosis Urgent Care Evaluation Initial Management and Stabilization Airway Assessment Anaphylaxis History Physical Examination Diagnostic Studies Imaging Studies Treatment Pharmacologic Treatment Pharmacologic Treatment for Histamine-Mediated Angioedema Epinephrine Antihistamines Corticosteroids Pharmacologic Treatment for Bradykinin-Mediated Angioedema Controversies and Cutting Edge Leukotriene Receptor Antagonists Tranexamic Acid Disposition Summary Time- and Cost-Effective Strategies Risk Management Pitfalls in Management of Angioedema in Urgent Care KidBits: Angioedema in Pediatric Patients Differential Diagnosis Urgent Care Management KidBits References Case Conclusions Coding & Charting: What You Need to Know Number and Complexity of Problems Addressed Amount and/or Complexity of Data to be Reviewed and Analyzed Risk of Complications and/or Morbidity or Mortality of Patient Management Abstract Patients experiencing angioedema commonly self-direct to urgent care centers. While acute presentations are often transient and localized, angioedema is a potentially life-threatening event that can rapidly progress to acute airway compromise, anaphylaxis, or both. Urgent care clinicians must quickly recognize the clinical presentations that indicate the need for emergency intervention. This article reviews the etiology and pathophysiology of angioedema, including the distinct mechanisms of the primary forms of angioedema, and presents evidence-based recommendations for the evaluation, treatment, and disposition of patients with angioedema in the urgent care setting. Case Presentations
CASE 1
A 52-year-old man presents to the urgent care clinic with a complaint of itching on his mouth and lips 20 minutes after biting into a doughnut at a local bakery... The symptoms started approximately 3 hours prior to his arrival at the clinic. He did not use his epinephrine autoinjector. He denies any shortness of breath. He states that he has a peanut allergy and has had similar reactions when he has eaten peanuts in the past, but he is certain there were no peanuts in or on his doughnut. Due to the risk of anaphylaxis associated with peanut allergies, the patient is prioritized for evaluation immediately after triage. He denies any new medications, chemical exposures, fevers, or exposure to animals or plants. He has not taken any NSAIDs and is not on an ACE inhibitor. His vital signs are: temperature, 36.4°C; heart rate, 76 beats/min; blood pressure, 123/84 mm Hg; respiratory rate, 14 breaths/min; and oxygen saturation, 98% on room air. On examination, his airway is patent. Mild symmetric swelling to the lips is noted. The oropharynx is unremarkable, and the uvula is midline and without swelling. There is a faint expiratory wheeze throughout lung fields. There is no visible rash, but dermographia is noted with a scratch test. You wonder how you should manage this patient...
CASE 2
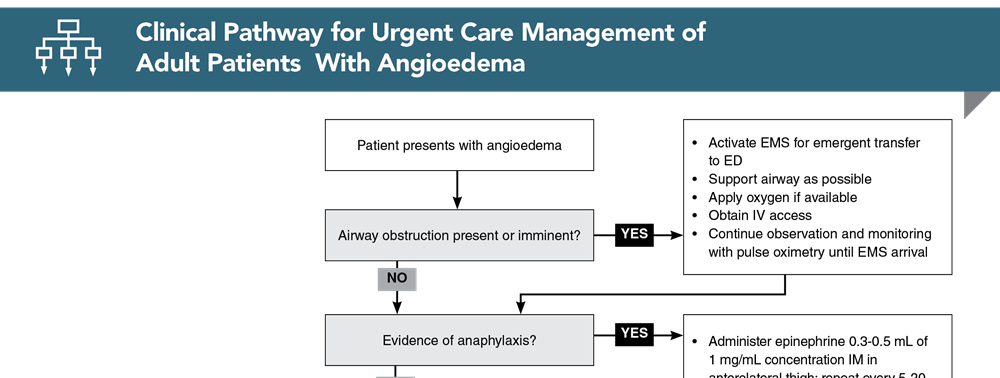
A 48-year-old woman presents to the urgent care clinic with lip swelling... She states her lips felt “heavy” when she woke up around 8 hours ago. She says her lips are significantly swollen, but the swelling has neither worsened nor improved. She denies shortness of breath, voice change, rash, itching, or prior history of similar occurrences, as well as fever or infection, any known allergies, or significant family history. She said she has had no recent exposures, travel, or trauma. The patient’s past medical history includes hypertension, diabetes mellitus type 2, and hyperlipidemia. She reports that she currently takes lisinopril, metformin, and atorvastatin. Her vital signs are: temperature, 37°C; heart rate, 82 beats/min; blood pressure, 138/78 mm Hg; respiratory rate, 16 breaths/min; and oxygen saturation, 100% on room air. On examination, the patient is in no distress, but she has significant upper and lower lip swelling, with no oropharyngeal involvement. The rest of her examination is unremarkable. You wonder if you should administer an antihistamine... How would you manage these patients? Subscribe for evidence-based best practices and to discover the outcomes. Clinical Pathway for Urgent Care Management of Adult Patients With Angioedema
Click to View the Interactive Pathway
Subscribe to access the complete Clinical Pathway to guide your clinical decision making. Key ReferencesFollowing are the most informative references cited in this paper, as determined by the authors. 1. * Macy E. Practical management of new-onset urticaria and angioedema presenting in primary care, urgent care, and the emergency department. Perm J.2021;25(4)1-7. (Review) DOI: 10.7812/TPP/21.058 4. * Long BJ, Koyfman A, Gottlieb M. Evaluation and management of angioedema in the emergency department. West J Emerg Med.2019;20(4):587-600. (Review) DOI: 10.5811/westjem.2019.5.42650 6. * Depetri F, Tedeschi A, Cugno M. Angioedema and emergency medicine: from pathophysiology to diagnosis and treatment. Eur J Intern Med.2019;59:8-13. (Review) DOI: 10.1016/j.ejim.2018.09.004 12. * Bernstein JA, Cremonesi P, Hoffmann TK, et al. Angioedema in the emergency department: a practical guide to differential diagnosis and management. Int J Emerg Med.2017;10(1):15. (Review) DOI: 10.1186/s12245-017-0141-z 19. Memon RJ, Tiwari V. Angioedema. In: StatPearls [Internet]. StatPearls Publishing. Updated August 8, 2023. Accessed February 15, 2024. (Online textbook chapter) 48. Farkas J. Angioedema. The Internet Book of Critical Care. Updated August 5, 2021. Accessed February 10, 2024. (Online textbook chapter) Subscribe to get the full list of 50 references and see how the authors distilled all of the evidence into a concise, clinically relevant, practical resource. Keywords: histamine, bradykinin, allergy, anaphylaxis, edema, swelling, pruritis, itching, urticaria, ACE inhibitor, airway, stridor, epinephrine, cetirizine, corticosteroids
Publication Information Author Lorilea Johnson, FNP-BC, DNP Peer Reviewed ByTracey Quail Davidoff, MD, FCUCM; Robert K. Beam, MD, PhD, FAAFP; Eric Macy, MD, MS, FAAAAI Publication DateMay 1, 2024 CME Expiration Date May 1, 2027
CME Information CME Information Date of Original Release: May 1, 2024. Date of most recent review: April 10, 2024. Termination date: May 1, 2027. Accreditation: EB Medicine is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians. Credit Designation: EB Medicine designates this enduring material for a maximum of 4 AMA PRA Category 1 CreditsTM. Physicians should claim only the credit commensurate with the extent of their participation in the activity. Specialty CME: Included as part of the 4 credits, this CME activity is eligible for 1 Pharmacology CME credit, subject to your state and institutional requirements. AAFP Accreditation: The AAFP has reviewed Evidence- Based Urgent Care and deemed it acceptable for AAFP credit. Term of approval is from 11/01/2023 to 10/31/2024. Physicians should claim only the credit commensurate with the extent of their participation in the activity. This session, Evidence-Based Management of Angioedema in Urgent Care, is approved for 4.0 enduring material AAFP Prescribed credits. AOA Accreditation: Evidence-Based Urgent Care is eligible for 4 Category 2-B credit hours per issue by the American Osteopathic Association. Needs Assessment: The need for this educational activity was determined by a practice gap analysis; a survey of medical staff; review of morbidity and mortality data from the CDC, AHA, NCHS, and ACEP; and evaluation responses from prior educational activities for urgent care and emergency medicine physicians. Target Audience: This internet enduring material is designed for physicians, physician assistants, nurse practitioners, and residents in the urgent care and family practice settings. Goals: Upon completion of this activity, you should be able to: (1) identify areas in practice that require modification to be consistent with current evidence in order to improve competence and performance; (2) develop strategies to accurately diagnose and treat both common and critical urgent care presentations; and (3) demonstrate informed medical decision-making based on the strongest clinical evidence. CME Objectives: Upon completion of this activity, you should be able to: (1) assess and evaluate a patient with undifferentiated angioedema; (2) select therapeutic agents for histamine-mediated angioedema; and (3) determine the proper disposition of patients with acute angioedema. Discussion of Investigational Information: As part of the activity, faculty may be presenting investigational information about pharmaceutical products that is outside Food and Drug Administration approved labeling. Information presented as part of this activity is intended solely as continuing medical education and is not intended to promote off-label use of any pharmaceutical product. Disclosure: It is the policy of EB Medicine to ensure objectivity, balance, independence, transparency, and scientific rigor in all CME activities. All individuals in a position to control content have disclosed all financial relationships with ACCME-defined ineligible companies. EB Medicine has assessed all relationships with ineligible companies disclosed, identified those financial relationships deemed relevant, and appropriately mitigated all relevant financial relationships based on each individual’s role(s). Please find disclosure information for this activity below: PlannersTracey Quail Davidoff, MD (Editor-in-Chief): Nothing to Disclose FacultyLorilea Johnson, DNP (Author): Nothing to Disclose Anna Schlechter, MD (KidBits Content Author): Nothing to Disclose Bradley Laymon, PA-C (Coding Content Author): Nothing to Disclose Tracey Quail Davidoff, MD (Peer Reviewer): Nothing to Disclose Robert K. Beam, MD (Peer Reviewer): Nothing to Disclose Eric Macy, MD (Peer Reviewer): Nothing to Disclose Angie Wallace (Content Editor): Nothing to Disclose Commercial Support: This issue of Evidence-Based Urgent Care did not receive any commercial support. Earning Credit: Go online to and click on the title of the test you wish to take.When completed, a CME certificate will be emailed to you. Additional Policies: For additional policies, including our statement of conflict of interest, source of funding, statement of informed consent, and statement of human and animal rights, visit .Close CME Credits4 AMA PRA Category 1 Credits™. 4 AOA Category 2-B Credits. 4 AAFP Prescribed Credits Specialty CME Credits: Included as part of the 4 credits, this CME activity is eligible for 1 Pharmacology CME credit. Get Permission Log in Buy This Issue Subscribe
Content you might be interested in
|